Introduction
Welcome to the first in Treehouse Counseling’s upcoming blog series about eating disorders. Before future articles delve into the nitty gritty of diagnosis and treatment, there is a preliminary topic on the minds of many who find themselves with a challenging relationship with food: when is an eating disorder actually an eating disorder? Our society encourages a significant gray area when it comes to adequate nutrition, but there is a clinically-defined difference between common disordered eating patterns and the criteria of a true eating disorder. Knowing the difference can guide you in the direction of the right type of support. If you or a loved one experience difficulties with food, or if you’re simply interested in further education on an underdiscussed topic, please read on.
Jump to Part 2: Eating Disorder Subtypes.
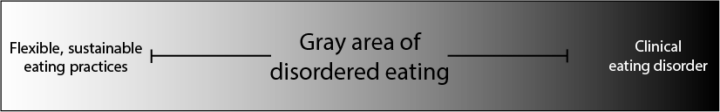
The Eating Disorder Spectrum
As with most diagnoses, the criteria required to meet a diagnosis of an eating disorder exist on a spectrum of severity. Some people live with one or two criteria, while others may live with all.
The spectrum below shows flexible, sustainable eating practices on the left (the term “healthy” is intentionally avoided here due to its subjectivity and tendency to include stigma) and clinical eating disorder on the right. That leaves a lot of gray area in the middle to make sense of. This is what we call disordered eating.
Disordered Eating Symptoms
Symptoms are often assessed by frequency and severity. With disordered eating, you may see many of the same behaviors that are present with an eating disorder, but often at a less severe level, and with less consistency. Below are some examples of disordered eating behaviors and mindsets to be aware of:
- Skipping meals or fasting (this does not include religious practices)
- Frequent changes in diet based on fads or social recommendations
- Restricting caloric intake
- Occasional binge eating or purging
- “Earning food” based on other compensatory behaviors like exercise
- Rigid food rules (when, how, why, what you can eat, etc.)
- Lacking a sense of control around food
- “Food noise” in your head (i.e. constant or frequent thoughts about food)
- Significant guilt or shame around food
- Basing your self-worth on the size or shape of your body
If these symptoms and experiences create significant medical instability or begin to take over the life and identity of the person in question, then an assessment for an eating disorder is recommended.
Meeting Diagnostic Criteria for an Eating Disorder
Eating disorder is the umbrella term for a category of several possible diagnoses, which we will go into further detail about in future articles. However, there are the core criteria to be aware of for any eating disorder.
Diagnostic Criteria per the DSM-5/ICD-10:
- Psychological impairment
- The preoccupation with food, weight, or body image is obsessive in nature and requires significant adjustments to lifestyle to accommodate
- Physical and social impairment
- Significant medical complications (not always visible externally)
- Unstable or orthostatic vitals (heart rate, and blood pressure); electrolyte imbalances; deterioration of teeth, nails, or hair
- Severely impairs social, occupational, or academic functioning
- Significant medical complications (not always visible externally)
- Frequency and severity of symptoms
- Behaviors occur often and with moderate to severe intensity
Disordered Eating vs Eating Disorder: A Comparison Chart
| Disordered Eating | Eating Disorder | |
| Intensity and Frequency of Symptoms | Occasional frequency, low to moderate intensity | Chronic and compulsive, moderate to severe intensity |
| Mindset | Preferential, comfort-based | Obsessive, all-consuming, coping-based |
| Life Impairment | Can cause stress on functioning | Causes significant impairment on multiple life areas (vocational, academic, social) |
| Medical Risk* | Lower immediate risk (e.g. no visible impact on vitals, no additional physical impairments) | Potentially severe medical complications (orthostasis, bone density, organ function, etc.) |
| Flexibility | May be able to bend or break food “rules” depending on circumstance | Inability to break routines without significant anxiety |
* This author chooses to emphasize the physical variability of human bodies. Some people develop physical signs of disordered eating immediately, while some can live with persistent eating disorders for decades and not manifest the same symptoms. Please do not judge the severity of someone’s potential eating disorder based solely on visible impacts, and instead defer to an eating disorder-trained medical professional.
When to Seek Support
When it comes to nutrition, any impact on our ability to nourish ourselves should be taken seriously. Disordered eating is not inherently better or less severe than a diagnosed eating disorder, and to perpetuate that idea is to send the incorrect message that someone may not deserve the support they are seeking.
Disordered eating is a warning sign. It is often progressive and impacts the body in ways that may go unnoticed without attention. Early intervention can be key in obtaining nutritional rehabilitation, breaking harmful thought-patterns, and learning new ways to cope with the stressors of life. If you have any concerns about your relationship to food and your body, help is warranted.
Future articles will go in-depth on models of treatment. For the time being, a few general suggestions:
- Talk to your primary care physician
- Consult with a therapist or a registered dietitian (or both!)
- When possible, always screen your providers for eating disorder training. Some providers still operate under outdated and fatphobic models of training, which may be the opposite of helpful
- Use a reputable online screening tool for preliminary information (links below)
Support can look a million different ways. If your curiosity brought you this far, then you are on the path to gathering more information about how to help yourself, your loved one, or to make change in society at large. It all starts with asking questions.
Thank you for reading, and take care.
Resources
Columbia River Eating Disorder Network – https://credn.org/
NEDA Screening Tool for Eating Disorders (ages 13 and up) – https://www.nationaleatingdisorders.org/screening-tool/
Citations
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.)
World Health Organization. (1993). The ICD-10 classification of mental and behavioural disorders. World Health Organization.